Meet the Regs (85 FR 25510)
CMS Prior Authorization Compliance with AI
Faster Response Times
Decision Recommendations
Audit-Proof Denial Reasons
Public Reporting
Decision Trees from Policy PDFs
Benchmark Policies Against Other Plans
Utilization Insights from Medical Models
Personalized PA Cost and Care Pathway Simulation
Streamline your utilization and case management with our AI automation. We use our own generative AI model built on patient histories to automate rule extraction from medical policies while better understanding of utilization management.
Prior Auth Automation & Compliance
Data Intake
- Extract structured patient data from all sources including faxes, HL7v2, C-CDA, FHIR and call centers transcripts
- Ingest medical policies from PDFs, web pages and portals
- Update daily or on change
By the brains that got 50+ plans compliant
Decision Support
- Generate determination decision recommendations for clinical review instantly
- Follow plan-specific workflows using coverage details and medical policies
- Automatically generate return letters
- Fully auditable citations for all approvals, denials and requests for more information
No manual logic, Our AI does the work
AI Review
- Generate provider gold card recommendations
- Get early abuse detection notifications
- Generate individual risk assessments per submission
- Identify next best action for care management
Human readable PA logic explanations
Save hundreds of hours of team time
Keep human-in-the-loop for final decision making while automating the time-consumingtasks of data extraction and coverage determination.Integrate directly into existing workflows
Our API-first approach allows for easy integration with existing EHR, claim processing, digital fax, case review or fileservers systems.Predict Care Pathways
Use GenHealth's Large Medical Model to generate optimal care pathway recommendations and next-best-action suggestions.Use our platform to transform PDFs to machine-readable rules in minutes.
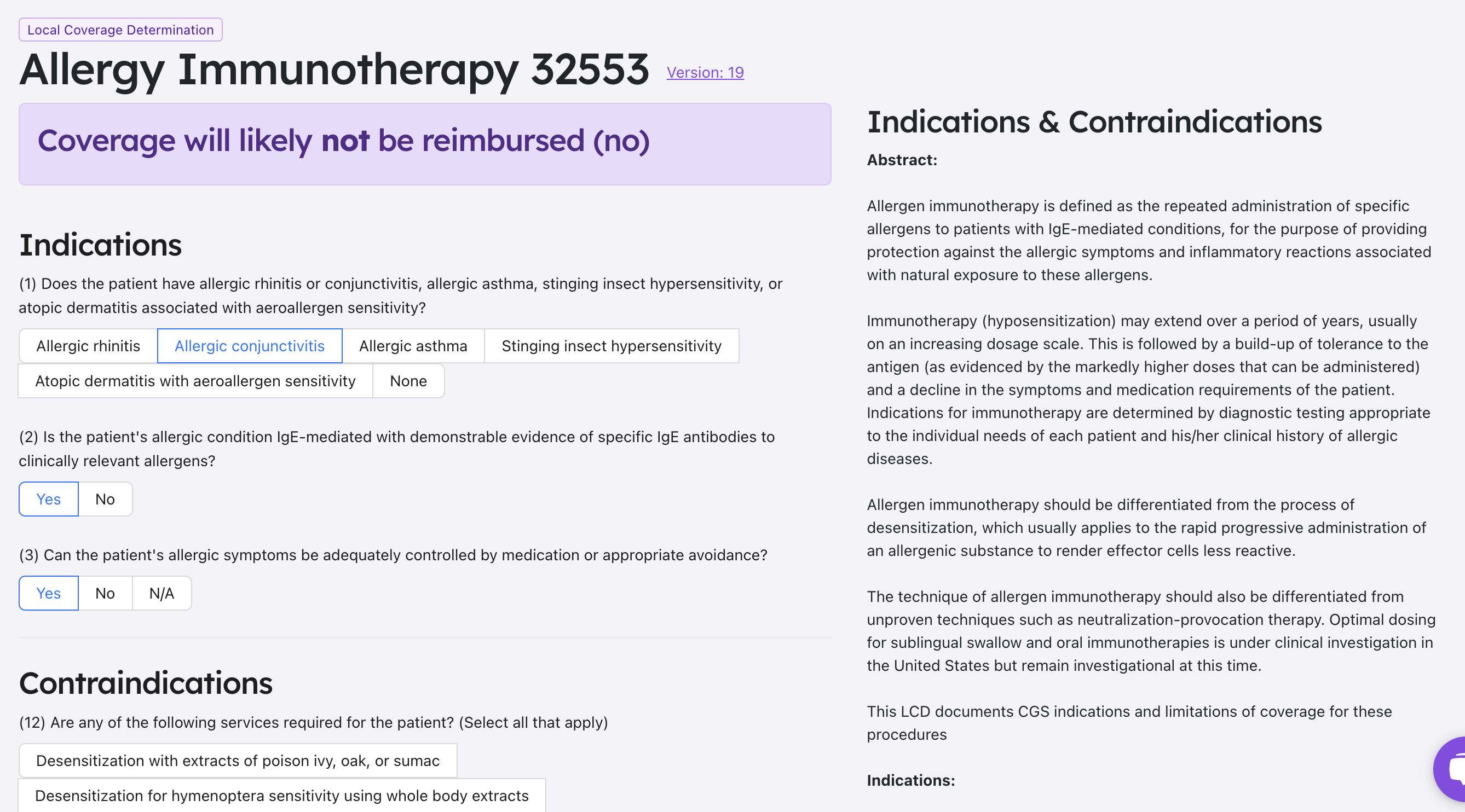
Take a look at our transformed Local and National Coverage Determinations from CMS. We've used our platform to generate easy-to-use, interactive questionnaires that can be used to generate accurate coverage recommendations, simplifying your decision-making process.